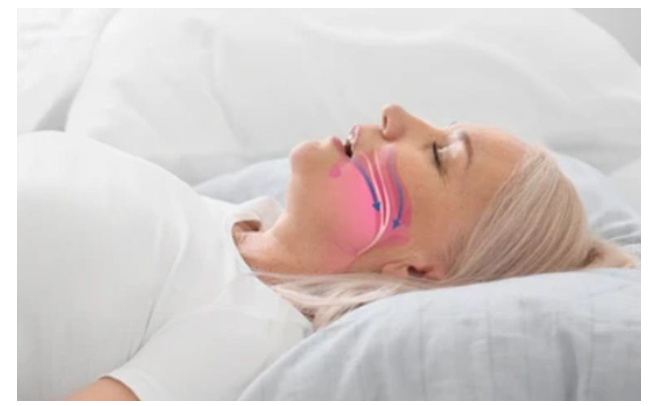
Obstructive sleep apnea (OSA) is characterized by obstructive apnea and hypoventilation caused by repeated collapse of the upper airway during sleep.
If you have OSA, what are the consequences of leaving it untreated?
l Excessive daytime sleepiness
l Impaired daytime function
l Metabolic dysfunction
l Increased risk of cardiovascular disease and death
OSA may also increase the risk of motor vehicle accidents and the possible negative results of driving or operating other dangerous equipment while drowsy.
What are the benefits of OSA treatment?
The goals of OSA treatment are to relieve signs and symptoms, improve sleep quality, and normalize apnea-hypopnea index (AHI) and oxygen saturation levels. The potential benefits of successful treatment of OSA include improved clinical performance (e.g., reduced daytime sleepiness), reduced health care service use and related costs, and possibly reduced cardiovascular complication rates and mortality.
What do OSA patients need to pay attention to in daily life?
Refrain from activities that require alertness and vigilance when sleepy.
Inform your doctor that you have sleep apnea, especially if you are planning surgery or on opioid medication.
Avoid alcohol as it may exacerbate OSA.
What should OSA patients be aware of in terms of medication?
In terms of medication, you should avoid certain drugs that have a depressant effect on the central nervous system. In particular, benzodiazepines should be avoided in untreated patients. Other medications that can exacerbate OSA and theoretically worsen daytime sleepiness include benzodiazepine agonists, barbiturates, other antiepileptics, sedative antidepressants, antihistamines, and opioids, especially antidepressants that can cause weight gain (e.g., mirtazapine).
What daily behaviors should be improved in OSA patients?
Encourage patients who are overweight or obese to lose weight and exercise; patients with postural OSA should change their sleep position accordingly, and avoid alcohol.
What are the most common treatments for OSA?
AASM, ATS, ACP, and the International Task Force on Geriatric Sleep Medicine all recommend positive airway pressure (PAP) ventilation as the initial treatment for all patients diagnosed with OSA in addition to behavior modification therapy.
The mechanism of CPAP machineis to maintain positive pharyngeal transmural pressure, thereby making pharyngeal transmural pressure greater than peripheral pressure. CPAP also stabilizes the upper airway by increasing end-expiratory lung volume, thereby preventing respiratory events (e.g., apnea, hypoventilation) due to upper airway collapse. Positive airway pressure therapy has the following benefits for OSA: Reduced frequency of respiratory events during sleep, reduced daytime sleepiness, improved body circulation blood pressure, reduced risk of crashing, improved erectile function and improved quality of life.
Are there other treatment options if I don’t want to use positive airway pressure therapy?
For patients with moderate OSA who do not want to use positive airway pressure therapy or for whom this therapy is ineffective, oral appliances (e.g., MAD, tongue retractors) are an alternative therapy that has been proven to improve symptoms and signs of OSA, and some patients may tolerate oral appliances better than positive airway pressure therapy.
In patients with severe OSA and/or severe sleep-related hypoxemia, the efficacy of oral appliances varies from person to person. Such patients are less suitable for oral appliances as primary therapy and positive airway pressure therapy can be more effective.
When is upper airway surgery necessary?
Several surgical approaches have been developed to treat OSA; surgery is usually considered when a patient refuses positive airway pressure or oral appliance therapy, or when therapy is ineffective (after at least 3 months of treatment).
Surgical treatment appears to be most effective if the patient’s OSA is caused by a severe upper airway obstructive lesion that can be surgically corrected, but positive airway pressure remains the first-line treatment for many patients with anatomic abnormalities of the upper airway. These lesions include tonsillar hypertrophy, adenoid hypertrophy, or craniofacial anomalies.